Ed Corrigan graduated from University of Maastricht before completing a Masters in Cancer, Stem Cells & Developmental Biology from Utrecht University. He has recently joined the Coffer Lab to work on a project focusing on understanding the biology and function of CD4+ effector T (Teff) cells in Juvenile Idiopathic Arthritis.
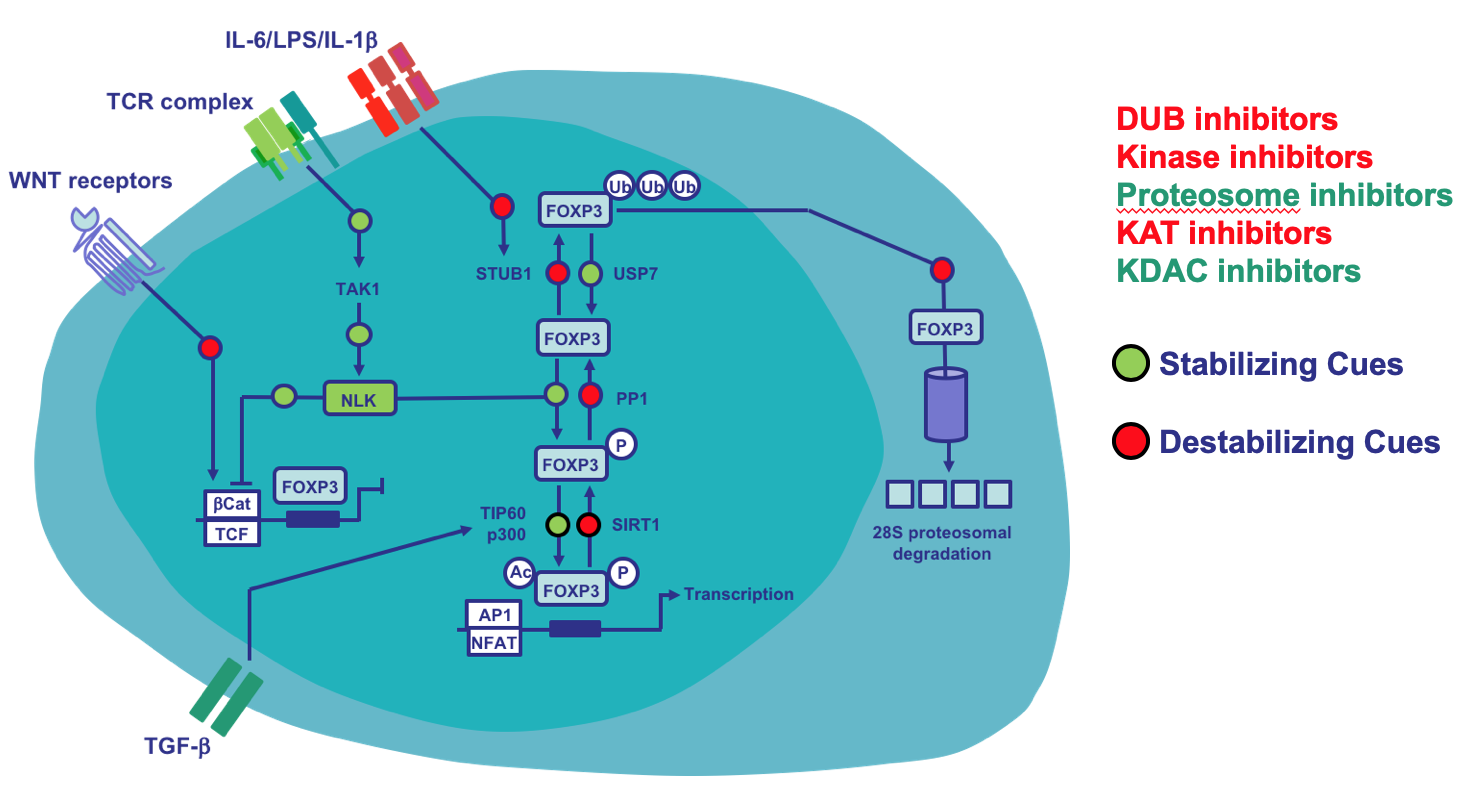
Juvenile idiopathic arthritis (JIA) is a chronic autoimmune disease affecting up to 1/1000 children in Western countries. Like many autoimmune diseases, it is caused by a loss of tolerance whereby inappropriately active T lymphocytes (T cells) in the joint help to generate a perpetuating inflammatory environment. One critical control mechanism that ensures that peripheral T cells avoid inappropriate activation is the induction of anergy. Anergy is defined as a state of unresponsiveness induced by suboptimal T cell stimulation from engagement of the T cell receptor (TCR) in the absence of co-stimulation. TCR activation without co-stimulation leads to a hyporesponsive state termed anergy, where cells not proliferate or produce cytokines, and are resistant to subsequent stimulation. Recent studies have expanded our understanding of the complex set of inputs that T cells integrate to determine their fate and engage in effector functions or become anergic. Interestingly, we have found that T cells isolated from the synovial fluid of JIA patients are resistant to anergy. In collaboration with the Macian Lab (Albert Einstein, NYC) we are the first to show a connection between autophagy and anergy. Whereas T cells that are allowed to induce autophagy become activated and primed to respond to subsequent stimulations, cells where activation-induced autophagy is prevented become anergic and show markedly reduced responses to re-stimulation. Importantly, inhibition of autophagy during T cell activation can lead to an ‘anergy-like’ long-lasting state of hyporesponsiveness.
In this project Ed will be examining the link between resistance to anergy and autophagy in JIA T cells, and evaluating relevance for disease pathogenesis and therapeutic intervention.
This work is supported by a grant from the Dutch Arthritis Foundation.