We are seeking an ambitious and talented postdoctoral scientist to join an exciting new ZonMw-funded project that aims to unravel how intracellular metabolism and transcription co-regulate embryonic development. This multidisciplinary research project brings together the complementary expertise of three Dutch institutes: the Coffer Lab (CMM, UMC Utrecht), the Sonnen Lab (Hubrecht Institute), and the Bauer Lab (TU Delft), offering a unique opportunity to work at the interface of developmental biology, biochemistry, and systems modeling.
Project Overview
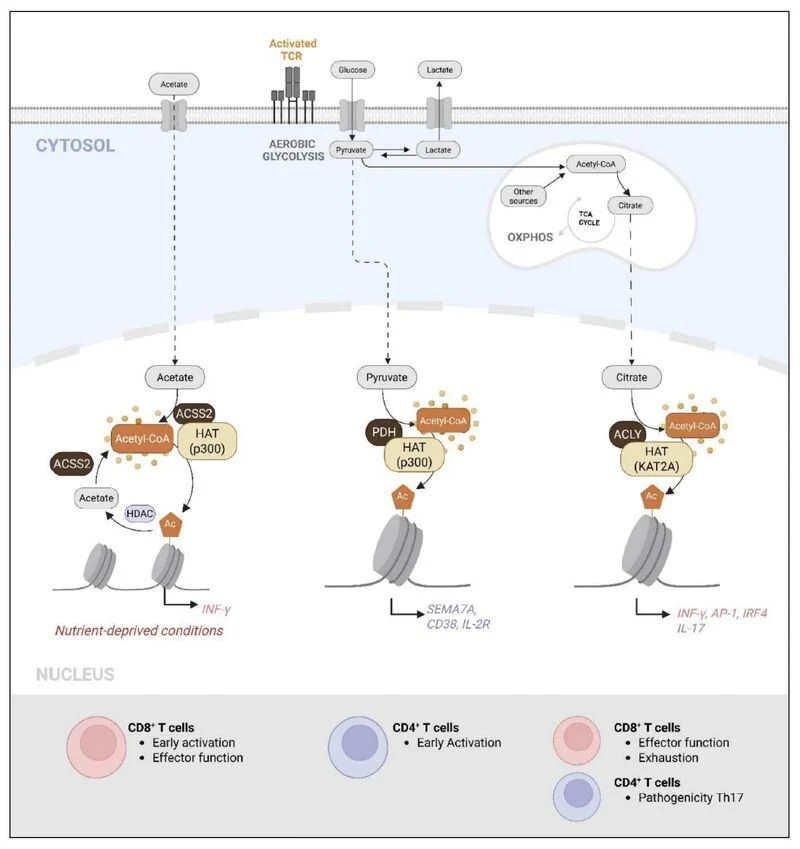
Titled “Signal Symbiosis: Exploring the Co-Regulation of Metabolism and Transcription in Embryonic Cell Fate”, this project investigates how nuclear metabolic enzymes influence transcriptional reprogramming during mammalian somitogenesis. The research focuses on metabolic signaling pathways (glycolysis and acetyl-CoA generation), their nuclear partitioning, and how they interact with dynamic developmental signaling circuits such as Wnt and Notch.
Using cutting-edge approaches—ranging from live cell imaging and metabolic biosensors, to proximity labeling and epigenomic profiling—the successful candidate will help uncover how nuclear metabolic events directly control gene expression and cell fate decisions in embryonic tissues and stem cell-derived organoid models.
The Position
The postdoctoral scientist will be based in the Coffer Lab at UMC Utrecht, a group with expertise in transcriptional regulation, metabolic control, and chromatin remodeling. You will collaborate closely with the Sonnen Lab, a leader in live imaging and microfluidic modeling of embryonic development, and the Bauer Lab, which brings quantitative systems biology and computational modeling expertise.
The successful candidate will take the lead in developing and applying novel biochemical tools to dissect nuclear metabolic complexes and their impact on chromatin state and transcriptional outcomes in developmental models.
Required Skills & Expertise
We are looking for a motivated and independent researcher with:
A PhD in molecular biology, biochemistry, developmental biology, or a related field;
Demonstrated experience with chromatin biology, transcriptional regulation, or metabolism;
Strong molecular and cellular technical skills
Experience with stem cell differentiation or 3D organoid models is an asset;
Excellent communication skills and a collaborative mindset, ideally with experience in multidisciplinary projects.
What We Offer
A dynamic, collegial environment at the Center for Molecular Medicine;
Access to state-of-the-art technologies and expertise across three partner institutes;
Mentorship, career development support, and the opportunity to co-supervise junior researchers;
A full-time, fixed-term appointment with competitive salary and benefits, in accordance with Dutch academic standards.
Interested?
For more information or to apply, please contact Prof. Paul Coffer (pcoffer@umcutrecht.nl) with your CV, a cover letter outlining your research interests and connection with the project goals. Review of applications will begin immediately and continue until the position is filled.